Abstract
Introduction: Although multiple myeloma (MM) is not considered an AIDS-defining malignancy such as certain types of non-Hodgkin lymphoma and Kaposi sarcoma, HIV infection can increase the risk of developing MM at a younger age. However, no robust data demonstrates that HIV infection could affect MM outcomes. Case reports or case series suggest that HIV positive MM has more aggressive biological features, clinical course, and shorter overall survival (Faure I et al, AIDS, 1999; Patra SK et al, J Clin Diagn Res, 2015). Other observational studies also reveal that HIV positive MM involves a younger population and has more extramedullary disease however survival data is yet to be explored (De Groot JJB et al, S Afr Med J, 2017; Giri S et al, Blood, 2018).
NYC has only 3% of the US population but has reported nearly 16% of all AIDS cases and the Bronx carries the highest HIV infection rate among all the boroughs (NYC Department of Health and Mental Hygiene, 2021). Based on that, we initiated a retrospective study in a tertiary medical facility in the Bronx to investigate the relationship between HIV infection status and the outcome of MM.
Methods: Using the electronic medical record data extraction software, we identified patients older than 18 diagnosed with HIV and MM between April 2009 and April 2022. HIV negative MM patients matched for age and ethnicity were included as control group. We conducted a retrospective chart review collecting demographic, laboratory and clinical characteristics and compared them between HIV positive and negative groups. Outcome data included response to initial therapy, presence of extramedullary disease, need for hospitalization during therapy, infectious complications, progression-free survival (PFS) and overall survival (OS). Statistical analysis was performed using chi-square testing for categorical variables and Mann-Whitney for continuous variables given the size of our sample.
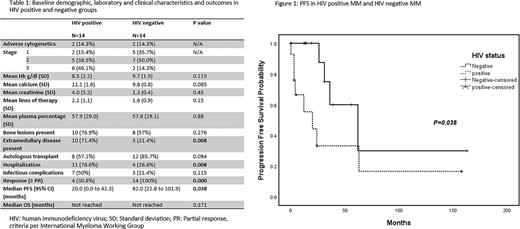
Results: A total of 14 patients were identified as HIV positive MM. 12 patients were on antiretroviral therapy, 2 patients were considered "long term non-progressor" who did not require treatment. In HIV positive group, mean CD4 count was 554 (71)cells/µl and mean viral load was 2477 (1634)copies/ml. The mean age on diagnosis was 61.5 years old (range 56-72), 57.1% patients were male (8/14), 100% of patients were African American. 9 had IgG subtype, 2 had IgA subtype, 2 had light chain subtype. International Staging System (ISS) stage 1, 2 and 3 were seen in 14.3% (2/14), 35.7% (5/14), 42.9% (6/14) patients, respectively. In one patient stage was unknown. Adverse risk cytogenetics were seen in 2 out of 13 patients at diagnosis (both were gain 1q). Cytogenetic information was not available in one patient. Mean number of lines of therapy was 2.1 and 8 out of 14 underwent autologous stem cell transplantation. Subsequently, 14 HIV positive patients were compared with 14 age/ethnicity-matched HIV negative patients with multiple myeloma. Median duration of follow up was 24 months (range 3-156) in HIV positive patients and 35 months (range 2-168) in HIV negative patients. No statistically significant differences were seen between the two groups in hemoglobin level, creatinine, calcium, lines of therapy, bone marrow plasma cell percentage, presence of bone lesions, number of lines of therapy, number of patients receiving autologous transplant, infectious complications, and OS (Table 1). HIV positive patients had significantly more extramedullary disease (71.4% vs. 21.7%, p=0.008), were hospitalized more often (78.6% vs 28.6%, p=0.008), had inferior response to induction therapy (21.4% vs 100%, p=0.001) (Table 1) and a shorter PFS (median 62.0 (95% CI, 22.8 to 101.9) months vs median 20.0 (95% CI, 0.0 to 42.3) months, p=0.038) (Figure 1).
Conclusion: Our study is the first single-center retrospective study evaluating the outcomes and prognosis of MM in minority patients with HIV infection. Despite well-controlled HIV infection with preserved CD4 counts, suppressed viral load and low risk disease in most HIV positive patients, they had more aggressive clinical course with more extramedullary disease, higher hospitalization rate, inadequate response to induction therapy and a shorter PFS compared with age and ethnicity matched HIV negative controls with multiple myeloma.
Disclosures
Murakhovskaya:Sanofi: Consultancy, Research Funding; Alexion: Research Funding; Rigel: Consultancy, Research Funding; Annexon: Research Funding; Kezar: Research Funding; Incyte: Research Funding; Novartis: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal